In Mozambique, where 11.5 percent of people between 15 and 49 years old live with HIV, conflict, stigma, and lack of adequate shelter can prevent people from accessing the treatment they need. Doctors Without Borders/Médecins Sans Frontières (MSF) staff are working not only to treat HIV but to create a supportive environment that breaks down barriers to care.
The ongoing crisis in Cabo Delgado, northeastern Mozambique—where armed conflict has been ongoing since 2017—has severely disrupted health care services, limiting access to HIV treatment for thousands. People face multiple challenges, such as restricted access to health care, shortages of antiretroviral (ARV) medications, and interruptions in their treatment due to insecurity and forced displacement.
HIV stigma can be deadly
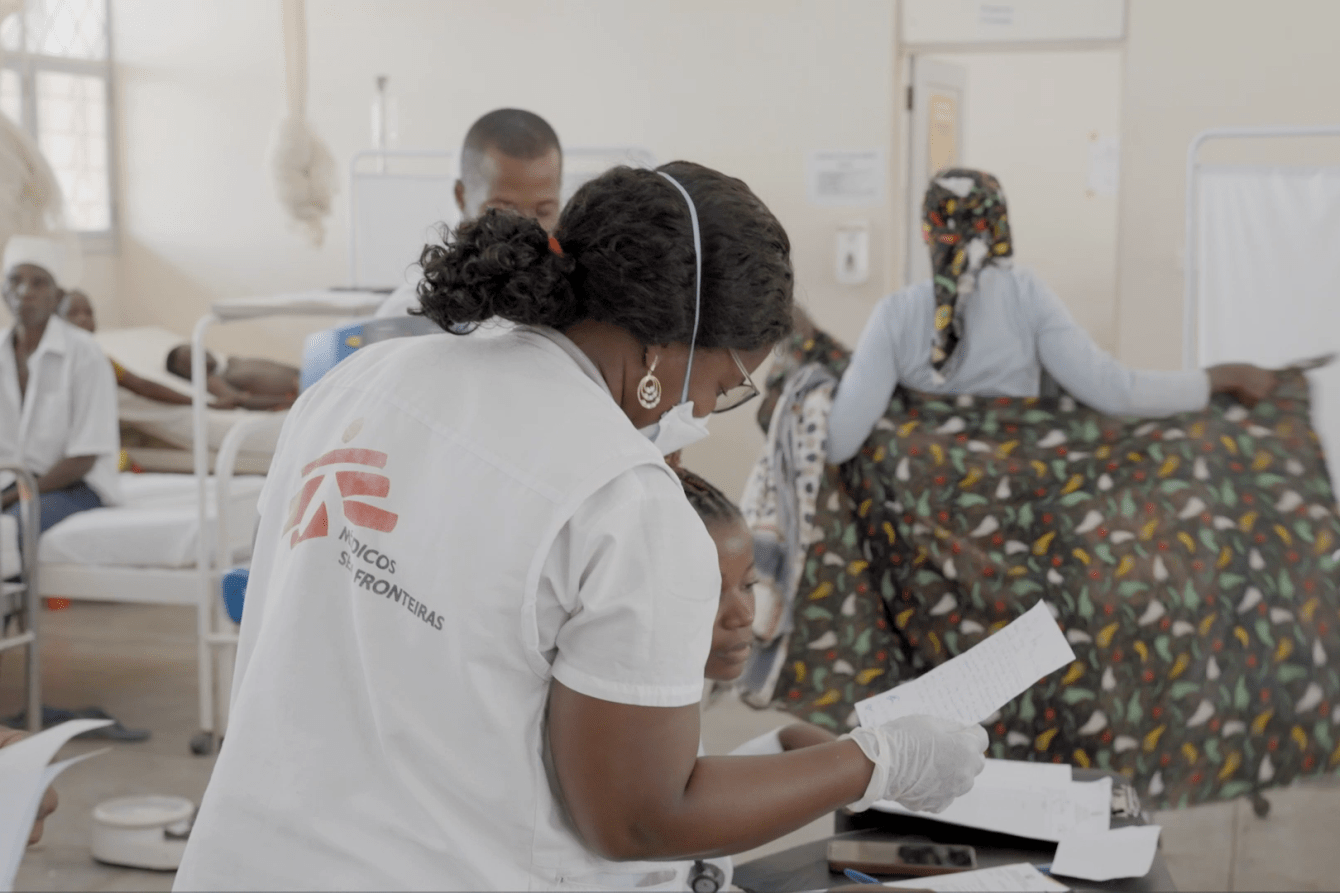
One focus of MSF’s work in Cabo Delgado is HIV care, which poses two major challenges, according to HIV specialist Dr. Filomena Januário: ensuring consistent follow-up care for patients displaced from their homes by violence, and addressing stigma within the community.
“I have always been passionate about medicine, but that passion deepened when my mother was diagnosed with diabetes and also contracted HIV,” says Dr. Januário. Fearful of other people’s judgement, her mother did not seek treatment for HIV and eventually died from complications associated with the disease. “She struggled to accept her diagnosis and sadly, she eventually lost her life,” says Dr. Januário. “That loss became my turning point. I promised myself: I will change this reality. I will dedicate my life to health so that I can care for my own family. Maybe if I had been a doctor [at the time], my mother’s life could have been saved.”
Through her work at the rural hospital in Mocímboa da Praia, Cabo Delgado province, Dr. Januário strives to ensure that no one else faces the same barriers her mother did to receiving lifesaving HIV care.

Conflict and displacement in Cabo Delgado
The ongoing violence in Cabo Delgado province has forced thousands of people to flee their homes. Many live in precarious conditions, with inadequate shelter, too little to eat, and poor sanitation—factors that exacerbate their vulnerability to infections, particularly for people whose immune systems are already weakened by HIV. Even when HIV care is available, stigma and discrimination deter many people from seeking treatment. For those who are on treatment, a lack of integrated care can make it hard for patients to stick to their ARV medication, which needs to be taken daily.
"One day, a patient is treated here, and the next day in another hospital, so the care is not integrated,” says Dr. Januário. “Many don't have a health care card and don’t know what medication they were taking or how long they had been taking it.”
“[Typically, patients] come to us because they relapsed,” adds Dr. Janúario. “We treat them, stabilize them, and restart their ARV treatment, but we don't know if they return to their place of origin. These patients are rarely retained in the program. Once in the advanced stages of HIV, patients without continuous treatment are more susceptible to stage 3and stage 4 infections.”

A mentor for expectant and new mothers
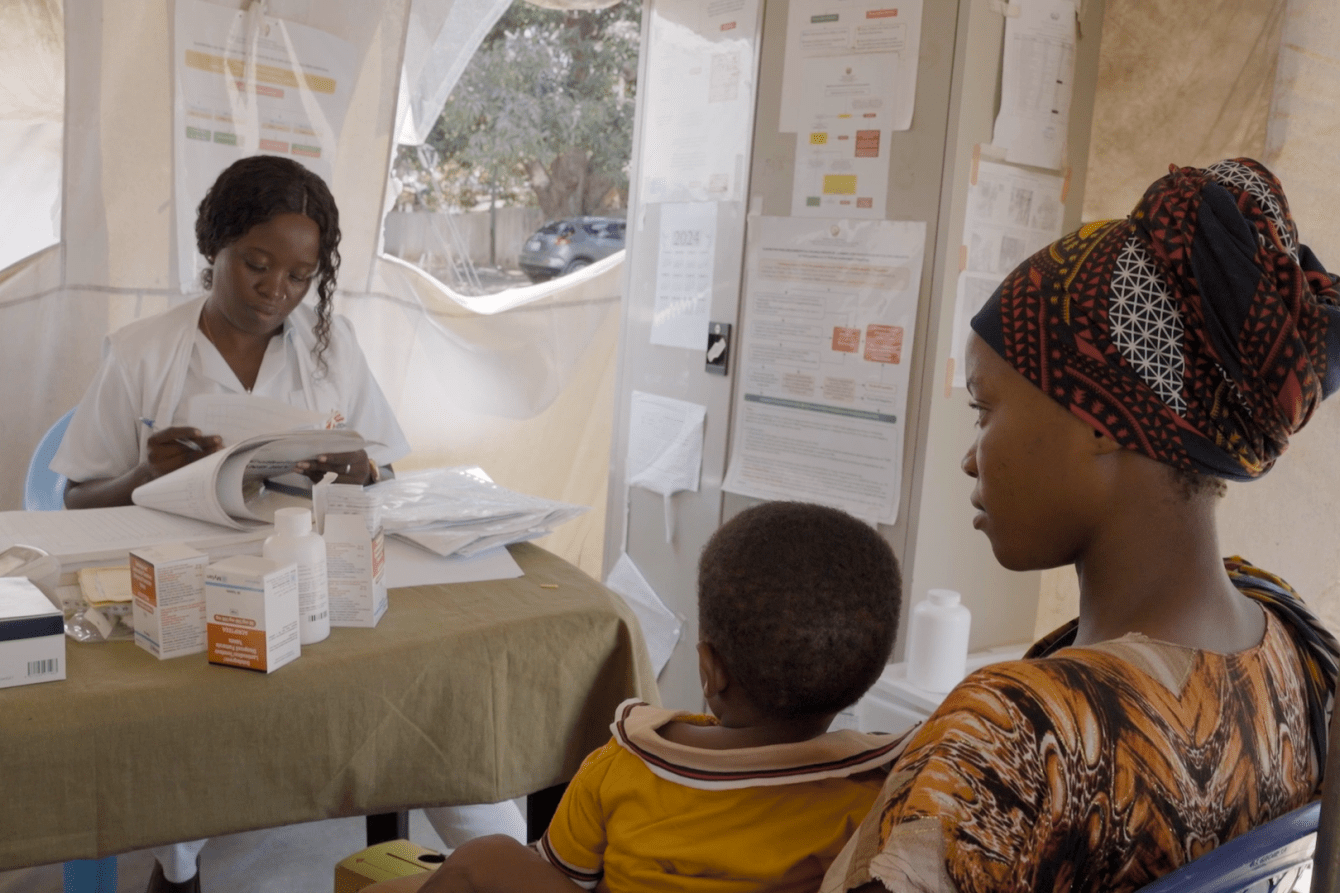
Working alongside Dr. Janúario is Cristina Virgílio, a mãe mentora (Portuguese for ‘mothers’ mentor’), who plays a vital role in preventing mother-to-child transmission of HIV. Virgílio runs awareness sessions for HIV-positive pregnant women and new mothers, encouraging them to seek support and stay on treatment.
Virgílio herself lives with HIV and shares her experience with other women, showing them that it is possible to bring up a family and live a healthy and happy life with the virus. Through this peer-to-peer approach supported by the Mozambican Ministry of Health, she helps build trust and dispel misconceptions about HIV, fostering a more inclusive and informed community.
"At first, when you receive the [HIV] diagnosis, it can be hard,” says Virgílio. “It’s important to support the person, reassure them, and show that this is not the end of the world. I’ve been living with HIV for many years. I’ve been taking my medication regularly and nothing serious has happened. I have children who were born healthy. For example, my daughter is HIV-negative, she’s growing up well, and this year she’ll turn 13. It’s possible to have healthy children when you follow the proper treatment.”
Germana Toni, who is receiving ARV treatment at Mocímboa da Praia rural hospital, found out she was HIV-positive when she first became pregnant. Receiving support from a mãe mentora was essential for her to keep up with her treatment throughout her pregnancy.
“[Virgílio] has always treated me with kindness and respect, offering valuable advice that motivates me to continue my treatment,” says Germana. “I encourage women and the community at large: If you test positive for HIV, it’s best to start treatment right away to ensure a healthy life.”
Building a supportive community
Working together, health care workers like Dr. Januário and Cristina Virgílio are making strides toward breaking down stigma and creating a safe environment for people affected by HIV. Their work highlights the importance of community-driven solutions in addressing both the medical and social challenges of HIV care in conflict settings.
However, Dr. Januário stresses that broader support is needed to ensure that every HIV-positive person affected by the conflict in Cabo Delgado can access consistent, lifesaving treatment. More resources and collective action are essential.
“I won’t be satisfied until we achieve a retention rate of over 80 percent [of patients staying on treatment], adds Dr. Januário. “I’m committed to doing everything possible to make that happen. Only then will I feel ready to leave Mocímboa da Praia, knowing I’ve reached my goal.”
Our work in Mozambique
Mozambique faces one of the highest HIV prevalence rates in the world. More than 2 million people are currently receiving ARV treatment, which is instrumental in reducing HIV-related transmission and deaths.
MSF has been working to bolster medical care and humanitarian aid for people in Cabo Delgado province since 2019. Working in partnership with the local Ministry of Health, MSF deploys medical staff, donates medications, and offers mental health support to displaced people and others affected by conflict.




