We receive many children with complicated cases of measles—more than I have ever experienced before in my life. Our hospital does not have an intensive care unit, so we refer patients who require mechanical ventilation to other hospitals. Sometimes caretakers tell me that they prefer to keep their children in our free-of-charge facility and leave the rest up to God’s will.
Although measles is a preventable disease, vaccination coverage among children being treated for measles is just 16 percent. Once the virus spreads in the community, morbidity and mortality can be high, especially among young children.
In the initial period of measles infection, symptoms are easy to miss or misdiagnose. Up until the fourth day, a patient exhibits flu-like symptoms: fever, cough, rhinitis, or a sore throat. After the fourth day, the patient develops telltale measles spots.
A sudden spike in cases
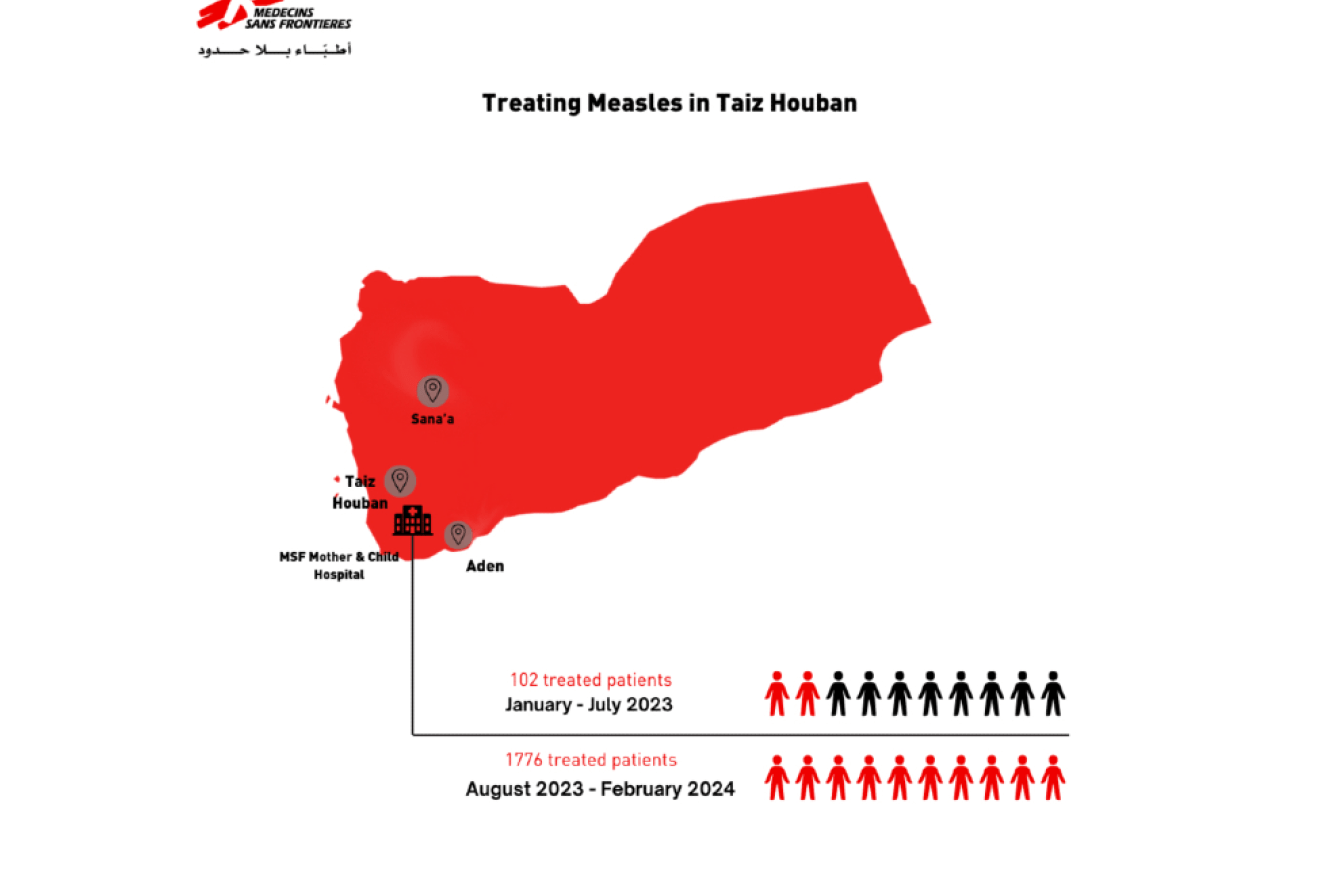
Measles is endemic to the area, and the hospital usually treats an average of eight measles patients each month. Last June, however, the numbers started to increase rapidly, with children from many districts in Taiz governorate arriving at the hospital.
Soon the number of measles patients had doubled. We could not risk cross-contamination in our wards, so in late August we decided to open a dedicated measles isolation unit. Six months later, the upsurge in measles cases shows no sign of abating and our efforts to address and contain the infection seem quite limited.

Children under five are particularly affected by measles since their immune systems are not sufficiently developed to withstand the infection. Once children contract measles, a temporary immunodepression causes measles-related infections such as pneumonia, conjunctivitis, inflammation of the ear and mouth, diarrhea, and swelling of the brain.
Access challenges
People in Taiz, much like in the rest of Yemen, struggle to access health care. The nearly decade-long conflict in Yemen has wrought a devastating toll on the country’s health infrastructure; many health facilities are either non-functional or are ill-equipped to cater to people’s needs. Added to this, basic health services in public health facilities are costly for the majority of people, whose financial capacity is quite constrained.
The lack of primary health care services pushes caretakers to delay bringing their sick children to the hospital in the hope that the symptoms will resolve on their own with home remedies or medication from their local pharmacy, if they have one. The long distances people must travel is an additional constraint, since most can barely afford the transportation costs.
Mother of an MSF patient
Ghadeer Abdel Rahman
My son complained of a fever, then had a seizure at home. He was breathing with difficulty and vomiting blood. It was late at night, and I was alone. I live in the frontline area where no one can travel at night. I was so scared. At sunrise, I rushed to the street and looked for transportation to the health center, but I could not afford the tests, as they were expensive.

There are, however, limitations to what the hospital can do when patients arrive at the hospital late in their sickness.
I will never forget Abdallah*, aged two-and-a-half, who was admitted to the measles unit at 7:30 p.m. one evening. He arrived with a rash, a fever, and huge ulcers around his mouth and lips. We suspected he had contracted diphtheria on top of his measles infection.
By 11:30 p.m., Abdallah was increasingly distressed and could not breathe well. At 12:30 a.m., he started to show signs of septic shock. We were preparing to transfer him to a governmental hospital where they treat diphtheria, but we worried that his body would not be able to handle the two-hour drive to go there.
At 3:30 a.m., he went into septic shock with signs of acute airway obstruction, so we intubated him to help him breathe better. Unfortunately, all these complications overwhelmed his body and Abdallah had a cardiopulmonary arrest. He did not survive. It shattered my heart.
Between August and December 2023, the MSF’s measles unit in the Taiz Mother and Child Hospital received 1,332 children, 85 percent of whom were under the age of four. In February 2024 alone, the unit received 220 measles patients. MSF’s epidemiological projections do not foresee a decrease in patient admissions anytime soon. If the transmission of measles is not contained, children in this area will continue to suffer a number of diseases that may become fatal if not properly treated in a timely manner.
*Names have been changed to protect privacy.




