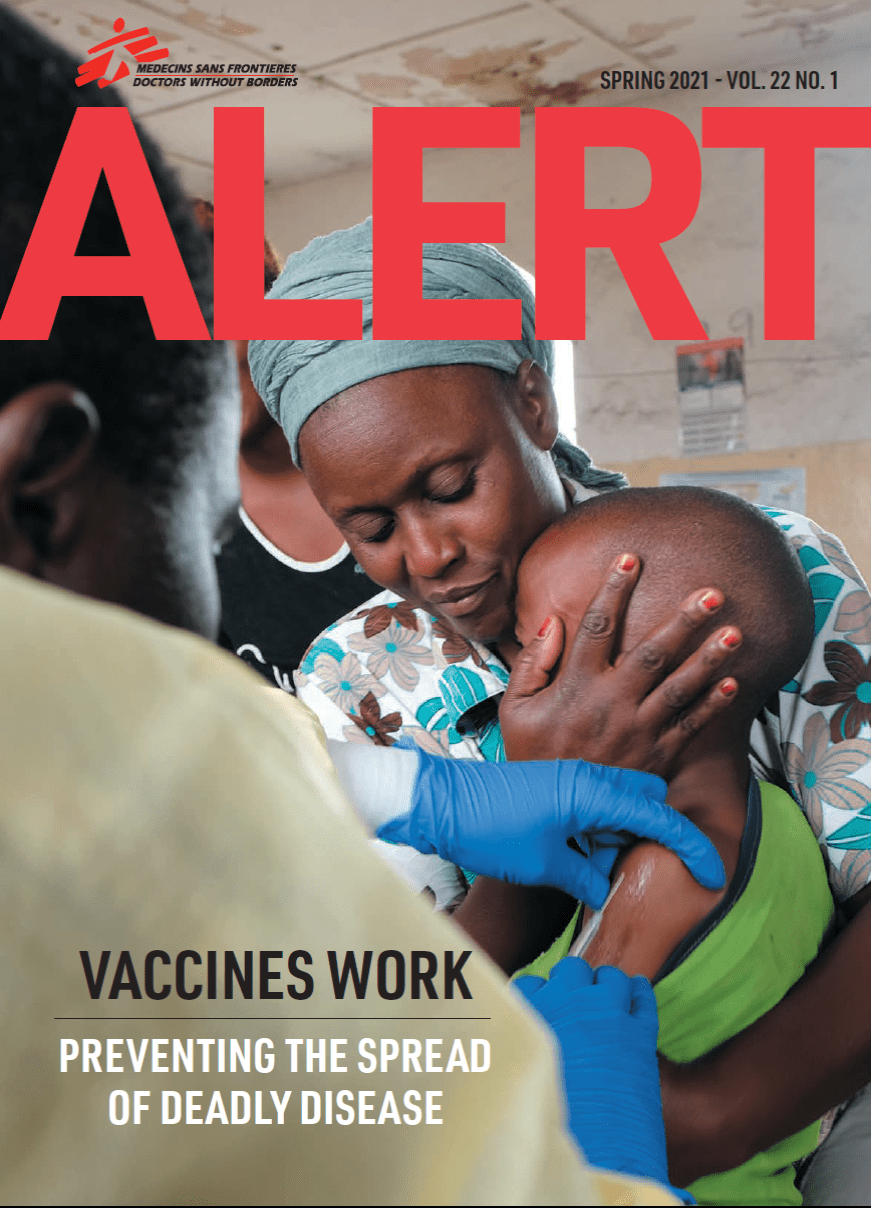
Doctors Without Borders/Médecins Sans Frontières (MSF) teams vaccinate millions of people every year in some of the world’s most challenging humanitarian contexts. Over the five decades that we’ve been running these campaigns, we’ve learned a lot, broken new ground, and consistently pushed for equitable access to vaccines. Here’s a look back at our work to get lifesaving vaccines to the people who need them most.
1972: MSF's first emergency response
Vaccination has been an integral part of MSF’s medical humanitarian work since its founding, when teams helped immunize children against measles during the organization’s first project in 1972 following the devastating earthquake in Managua, Nicaragua.
1986: MSF Logistique created

This MSF purchasing and supply center ensures that MSF teams on the ground have everything they need to respond quickly to outbreaks and other emergencies. Logistique develops standardized supply kits along with internationally recognized clinical guidelines. In 1988, the World Health Organization (WHO) adopts the concept with its “emergency health kit.” Vaccination kits developed for measles, meningitis, and yellow fever enable us to quickly set up a cold chain system to safely store doses.
1986: Epicentre founded
This MSF entity carries out epidemiological research and clinical trials during outbreaks and other humanitarian contexts. Epicentre regularly publishes findings in scientific journals to share data and analysis. Research on the use of fractional dosing, heat-stable vaccines, and preventive and outbreak response vaccination strategies can help us save more lives.
1996: Meningitis outbreak in Nigeria

To confront the largest meningitis outbreak ever recorded in Nigeria, MSF mounts a massive response supported by international staff and several tons of medical equipment. Nearly three million people are vaccinated against the disease and more than 30,000 cases are treated. While the scale of the response is impressive, it also leads to a worldwide shortage of vaccine stocks and questions about effectiveness.
1997: An international partnership
Based on lessons learned during the meningitis vaccination campaign in Nigeria, MSF, WHO, and other partners establish the International Coordinating Group (ICG) on vaccine provision for epidemic meningitis control. The ICG evaluates vaccine needs in meningitis belt countries alongside available resources to guarantee the rational use of supplies. This innovative public health action group becomes a model for coordinating the response to yellow fever and drug-resistant tuberculosis.
1999: Access Campaign is born

MSF’s Access Campaign is founded to advocate for available, affordable vaccines, drugs, and tests suited to the people we care for and adapted to the places where they live. In the years since, the Access Campaign has pushed for equitable access to HIV medicines, advocated for cheaper and more effective drugs to treat tuberculosis, and pushed corporations to drop the price of pneumonia vaccines. We're now calling for global equitable access to COVID-19 vaccines.
2004: Oral vaccines
In collaboration with WHO, Epicentre, and others, MSF helps pioneer the use of oral cholera vaccines to control an epidemic in Mozambique, which has long been plagued by outbreaks of the waterborne disease. Previously, cholera interventions had focused on improving infrastructure and hygiene services to prevent outbreaks. This new, proactive approach proves successful, and lays the groundwork for future cholera responses in regions where the disease is endemic.
2007: Pushing for vaccine equity

Pneumonia can be prevented with the pneumococcal conjugate vaccine (PCV), but pharmaceutical companies Pfizer and GlaxoSmithKline have a global monopoly, putting it out of reach of children in many countries. In 2007 MSF begins pushing Big Pharma to lower PCV prices, but they refuse, instead offering unreliable and unsustainable vaccine donations. This is the beginning of years of effort by MSF to address PCV vaccine inequity.
2010: MenAfriVac
MSF supports the ministries of health in Mali and Niger in implementing the distribution of MenAfriVac, a new meningitis vaccine that provides protection from the disease for up to 10 years and dramatically lowers the spread of meningitis A across sub-Saharan Africa.
2013: Pushing the limits of cold storage
An Epicentre study finds that a tetanus toxoid vaccine normally stored near freezing remains stable and effective when kept at controlled temperatures of up to 104 degrees Fahrenheit for up to 30 days. It paves the way for other vaccines to be used in places where maintaining a cold chain is difficult, and pressures pharmaceutical companies to re-label and share data on heat-stable vaccines.
2014: Ebola in West Africa

MSF responds to the largest-ever Ebola outbreak by sending medical teams to Guinea, Liberia, Sierra Leone, and Mali. We are part of the first trial of the now-approved Ebola vaccine in Guinea, publishing the findings in the New England Journal of Medicine in May 2015.
2015: A Fair Shot
On World Pneumonia Day, MSF launches a new campaign for more affordable PCV
vaccines. We start a global petition calling on Pfizer and GlaxoSmithKline to reduce the price of
the shot—the most expensive standard childhood vaccine—to $5 in low- and middle-income countries.
2016: Pioneering partial dosing

When a cholera outbreak strikes Zambia, MSF helps plan a campaign to vaccinate at least half a million people in the capital city of Lusaka. But the global emergency stockpile of the oral cholera vaccine is too low to supply the standard two doses per patient. To reach maximum coverage with limited supplies, MSF suggests providing single doses of the vaccine and distributing the second when more supplies became available, a strategy that had previously been proven effective. Nearly 1,700 volunteers work alongside 100 MSF and Ministry of Health staff to help implement the successful campaign. Partial dosing has since been used to curb disease outbreaks in diverse settings.
2017: The Humanitarian Mechanism

MSF, WHO, UNICEF, and Save The Children establish the Humanitarian Mechanism, which sets requirements for vaccine supplies in emergencies and allows humanitarian organizations to purchase vaccines from manufacturers at reduced prices during humanitarian emergencies.
2019: Vaccinating refugee children in Greece

The Humanitarian Mechanism is used for the first time in a high-income country as MSF vaccinates children stranded in refugee camps on the Greek islands of Chios, Samos, and Lesbos against pneumonia. The PCV vaccine normally costs $168 per child in Greece, but through the program MSF is able to obtain it for $9. Providing a lifesaving vaccine to refugee children in a country where they otherwise could not afford it is an important step, but until manufacturers make more affordable vaccines for childhood diseases the Humanitarian Mechanism remains a stopgap solution.
2021: Fractional doses for yellow fever
Epicentre publishes a study that shows administering just one-fifth of the standard vaccine dose for yellow fever—a mosquito-borne disease that kills nearly 30,000 people every year—is an effective and safe way to prevent the disease. Fractional dosage means that MSF and other health organizations can vaccinate more people in response to outbreaks.
2021: Ensuring supplies of Ebola vaccine
A global stockpile of the Ebola vaccine is created to ensure treatment providers like MSF have access to supplies in case of an outbreak. From 2018 to 2020 the vaccine was used during the tenth and largest Ebola outbreak in the history of Democratic Republic of Congo.
2021: No profiteering in a pandemic

MSF calls for no patents or profiteering on vaccines, drugs, or tests used during the
COVID-19 pandemic. We are demanding global equitable access to lifesaving coronavirus vaccines.